Reusable wearable sensor monitors Covid-19
As the initial peak of the Covid-19 pandemic passes, researchers are looking more closely at ways to monitor patients who might have the disease, first in hospital and now at home.
Researchers at Northwestern University and the Shirley Ryan AbilityLab in Chicago initially developed the wearable device to monitor the symptoms of a stroke, but are now creating a set of data algorithms to catch early signs and symptoms associated with Covid-19. This uses similar algorithms to the patient deterioration disposable patch developed by Philips that is now being used in a hospital in the Netherlands: WEARABLE BIOSENSOR MONITORS PATIENTS FOR EARLY DETERIORATION
About 25 affected individuals began using the Northwestern device two weeks ago and the researchers at the Ability Lab are using data from the clinic and at home to refine the algorithms.
Rather than relying just on temperature, the sensor monitors coughing intensity and patterns, chest wall movements (which indicate laboured or irregular breathing), respiratory sounds and heart rate. The data is wirelessly sent to a secure cloud, where automated algorithms produce graphical summaries to provide rapid, remote monitoring.
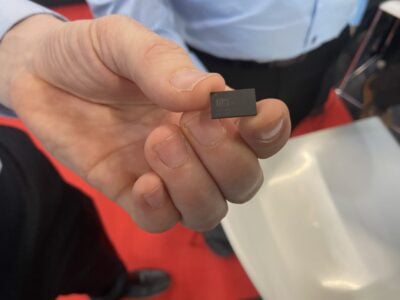
Because it is fully encased without wires, electrodes, charge ports or removable batteries, the wirelessly-charged device can be worn while exercising or in the shower. The sealed design is also important for sterilization and reuse.
“This is absolutely critical for use in the context of this extremely contagious disease,” said John Rogers at Northwestern Engineering who led the technical development. “Because it is fully sealed in a soft biocompatible silicone material, it can be completely immersed in alcohol, and then exposed to a gas-based system for rigorous sterilization. If there were exposed regions, or plugs or ports or other physical interfaces, the device would not be relevant for this application.”
“The most recent studies suggest that the earliest signs of a COVID-19 infection are fever, coughing, and difficulty in breathing. Our device sits at the perfect location on the body — the suprasternal notch — to measure respiratory rate, sounds, and activity because that’s where airflow occurs near the surface of the skin,” said Rogers. “We developed customized devices, data algorithms, user interfaces, and cloud-based data systems in direct response to specific needs brought to us by frontline healthcare workers. The measurement capabilities are unique to this device platform — they cannot be accomplished using traditional watch or ring-style wearables that mount on the wrist or the finger.”
“We anticipate that the advanced algorithms we are developing will extract Covid-like signs and symptoms from the raw data insights and symptoms even before individuals may perceive them,” said Arun Jayaraman, a research scientist at Shirley Ryan AbilityLab, who is leading the algorithm development. “These sensors have the potential to unlock information that will protect frontline medical workers and patients alike — informing interventions in a timely manner to reduce the risk of transmission and increase the likelihood of better outcomes.”
The device can monitor hospitalized patients and then be taken home to continue 24/7 supervision. The real-time data streaming from patients gives insights into their health and outcomes that is currently not being captured or analyzed by traditional monitoring systems.
“This opens up new telemedicine strategies as we won’t have to bring in patients for monitoring,” Jayaraman said. “Physicians can potentially review the patients’ data for hours, days, or weeks, immediately through a customized graphical user interface to a cloud data management system that is being set up for this purpose, to see an overall image of how the patient is doing.”
“As the algorithm becomes smarter, our hope is that it will begin to discriminate among which coughs are Covid-like and which are from something more benign,” Jayaraman said. “The most basic approach, already deployed on Covid-19 patients and health care workers, simply counts coughs and their intensity.”
The team is already producing dozens of devices per week. Rogers estimates that his team could produce up to hundreds of devices per week, all in house, largely bypassing the need for external vendors and complex supply chains.
In the coming weeks, the teams at Northwestern and Shirley Ryan AbilityLab will continue collecting patient data to strengthen their algorithms through deployments both in the clinic and at home. They also are responding to other requests for access to the technology in Chicago with additional deployments starting now.
The research group is at rogersgroup.northwestern.edu
Related Covid-19 articles
- CONNECTED BOLLARD FIGHTS VIRUS
- SKYWATER TO MAKE TEMPERATURE SENSOR FOR PATCH
- OPEN SOURCE MEDICAL EQUIPMENT REPAIR DATABASE
- WHITE PAPER EVALUATES VIRUS IMPACT ON KEY TECHNOLOGIES
 If you enjoyed this article, you will like the following ones: don't miss them by subscribing to :
eeNews on Google News
If you enjoyed this article, you will like the following ones: don't miss them by subscribing to :
eeNews on Google News